Authors:
Janna Kimel, Jay Lundell
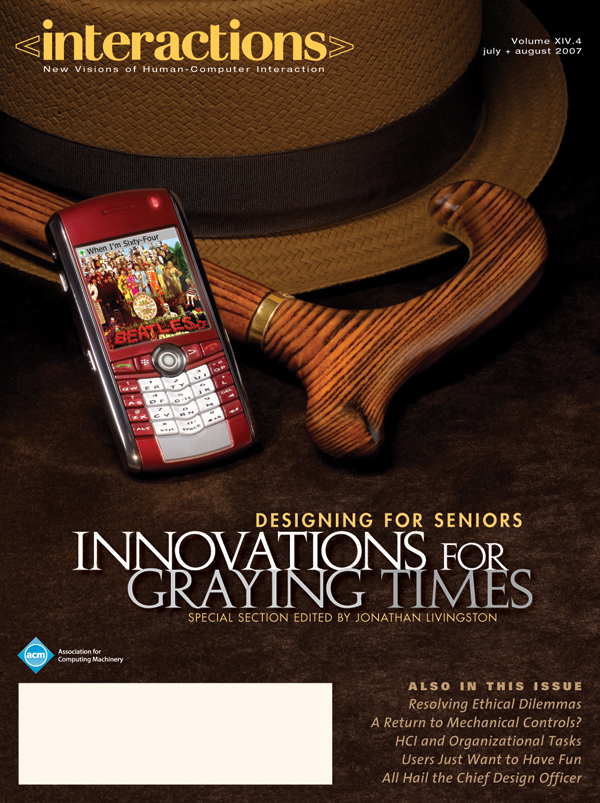
There is an increasing focus in industry and academia on developing technology to allow older people to remain in their homes for as long as possible [1, 6]. One approach involves "pervasive technology"the deployment of various sensors, computers, and output devices embedded in the home environment to track behavior and interactions with household objects (Figure 1). Behind the technology sits software that measures, for example, activities of daily living (ADLs), accumulates this information, and uses it to notify relatives or medical people of the status of an older person living alone [5]. Additionally, this software could provide direct assistance…
You must be a member of SIGCHI, a subscriber to ACM's Digital Library, or an interactions subscriber to read the full text of this article.
GET ACCESS
Join ACM SIGCHIIn addition to all of the professional benefits of being a SIGCHI member, members get full access to interactions online content and receive the print version of the magazine bimonthly.
Subscribe to the ACM Digital Library
Get access to all interactions content online and the entire archive of ACM publications dating back to 1954. (Please check with your institution to see if it already has a subscription.)
Subscribe to interactions
Get full access to interactions online content and receive the print version of the magazine bimonthly.





Post Comment
No Comments Found